

120 days after you first wrote to us, if we did not answer that request in some way within 30 days, or.90 days after the date of our letter upholding our initial decision, or.If you do not agree with our decision, you may ask OPM to review it. We will base our decision on the information we already have. If we do not receive the information within 60 days we will decide within 30 days of the date the information was due. You or your provider must send the information within 60 days of our request. Ask you or your provider for more information.Write to you and maintain our denial, or.In the case of a post-service claim, we have 30 days from the date we receive your request to: You may respond to that new evidence or rationale at the OPM review stage described in Step 4.
However, our failure to provide you with new evidence or rationale in sufficient time to allow you to timely respond shall not invalidate our decision on reconsideration. We will provide you with this information sufficiently in advance of the date that we are required to provide you with our reconsideration decision to allow you a reasonable opportunity to respond to us before that date.
#Aetna timely filing limit 2021 free#
#Aetna timely filing limit 2021 how to#
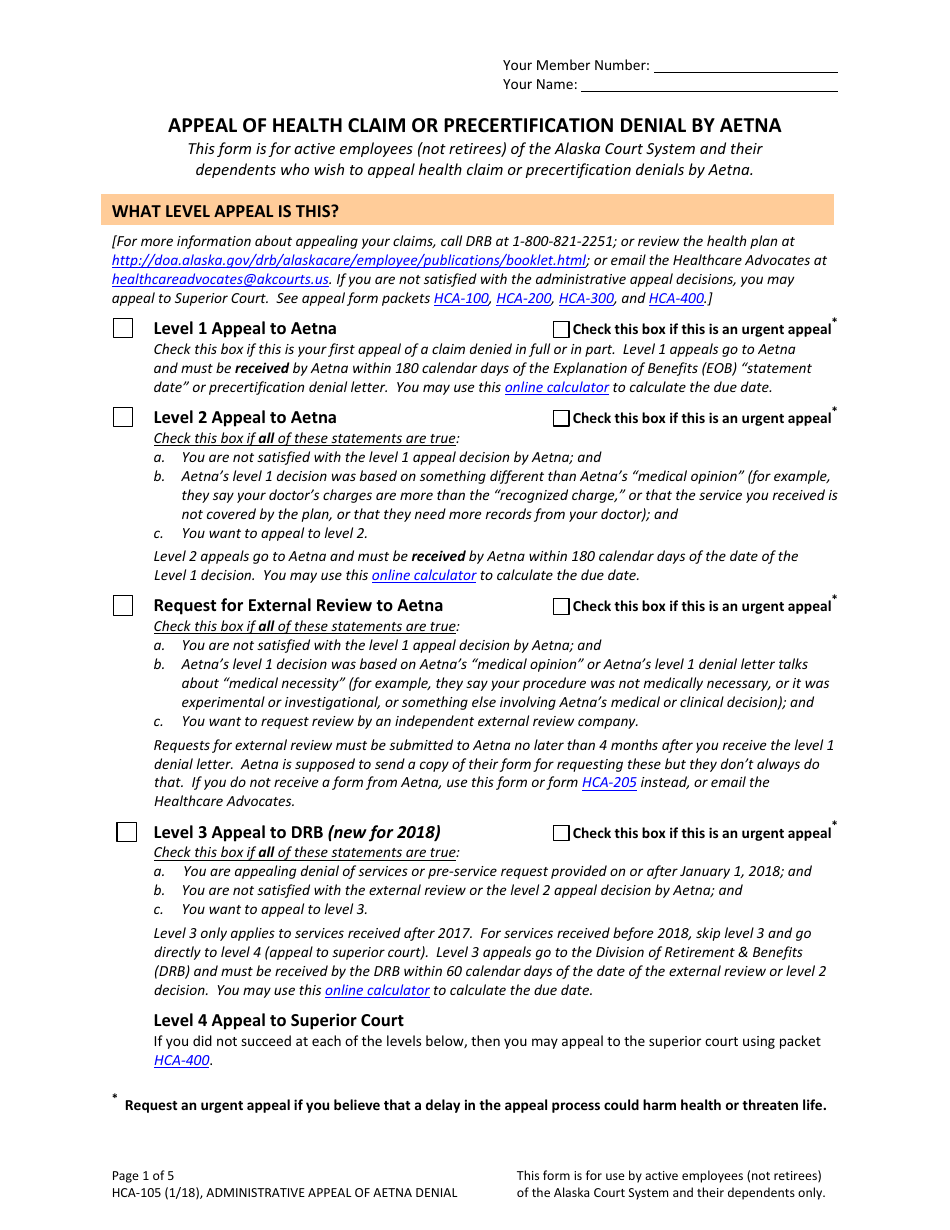
How to File an AppealĪsk us in writing to reconsider our initial decision. Follow this Federal Employees Health Benefits program disputed claims process if you disagree with our decision on your claim or request for services, drugs, or supplies, including a request for preauthorization/prior approval.


 0 kommentar(er)
0 kommentar(er)
